Every year, nearly half a million people in the United States are treated for burn injuries. The majority of initial burn care and evaluation occurs outside of a burn center environment, at local hospitals and clinics. Many providers struggle with when to manage a burn independently and when to refer to a specialist. Below, we cover initial assessment and referral guidelines for burned patients. The University Hospital Burn Center is available as a resource to you at all times.
Determining the severity of a burn
Burns are challenging to assess, particularly when the injury is new. These wounds tend to evolve over the first 48-72 hours after the injury. Often, the full extent of the damage to skin and underlying tissues is not clear.
The depth of a burn is dependent on the temperature of the heat source, duration of contact, thickness of the epidermis and dermis, and blood supply to the area of the burn. For example, very young and elderly patients have thinner skin and are more susceptible to deeper burns.
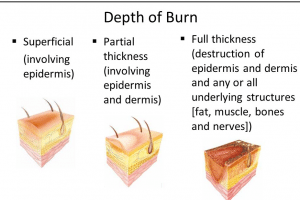
Characteristics of superficial, partial-, and full-thickness burns
• First degree (superficial) burns appear red, erythematous, and often painful. Sunburn-like presentation.
• Second degree (partial thickness) burns presentation includes redness, blistering and swelling. Very painful.
• Third degree burns (full thickness) appear whitish, charred, or translucent. No sensation to pin-prick in burned area. Minimal pain.
When to make a referral
The American Burn Association recommends referral to a burn center for the following patient situations:
1. Partial thickness burns greater than 10% total body surface area (TBSA)*
2. Burns involving the face, hands, feet, genitalia, perineum or joints
3. Suspected third degree burns, any age
4. Electrical burns, including lightning injury
5. Chemical burns
6. Inhalation injury
7. Burn injury in patients with other medical disorders that could complicate management, prolong recovery, or affect mortality
8. Any patient with burns and concomitant trauma (such as fracture) in which the burn injury poses the greatest risk to the patient. In such cases, if the trauma poses the greater risk, patients should be stabilized in a trauma center prior to transferring to a burn center. At UW Health, The Burn Center staff routinely partner to serve patients with burn and trauma injuries.
9. Burned children, any size burn, in hospitals without the resources to care for children
10. Burn injury in patients who require special social, emotional, or rehabilitative intervention
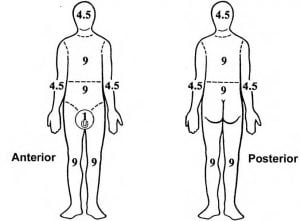
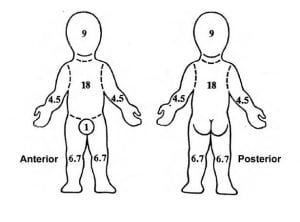
*TBSA can be estimated using the palm and fingers of the patient’s hand. One palm+fingers= approximately 1% TBSA. Always use the patient’s hand, not your own, to estimate TBSA.
*The Rule of Nines is another method of measuring burn size.
For more information or treatment:
The UW Health Burn Team is available to collaborate regarding patients at all times. Please contact the Access Center at (608) 263-3260 to reach us.
To schedule education or training about the evaluation and treatment of burn wounds, please contact Andrea Wipperfurth, Program Manager, at (608) 263-8024.
References
American Burn Association (2016). Advanced Burn Life Support Course, 2016 Update. Chicago, IL.
Committee on Trauma, American College of Surgeons (2006). Guidelines for the Operations of Burn Centers Resources for Optimal Care of the Injured Patient.
American Red Cross. Emergency Medical Response presentation. (burn depth image)